What is Pelvic Organ Prolapse?
Pelvic Organ Prolapse by definition is the descent of one or more of the walls of the vaginal canal. In other words, there is a laxity, weakness or increased stretch of the connective tissues that attach the digestive and reproductive organs together within the pelvis. Prolapse is consequently known as a supportive dysfunction and is often associated with poor pressure management within the body.
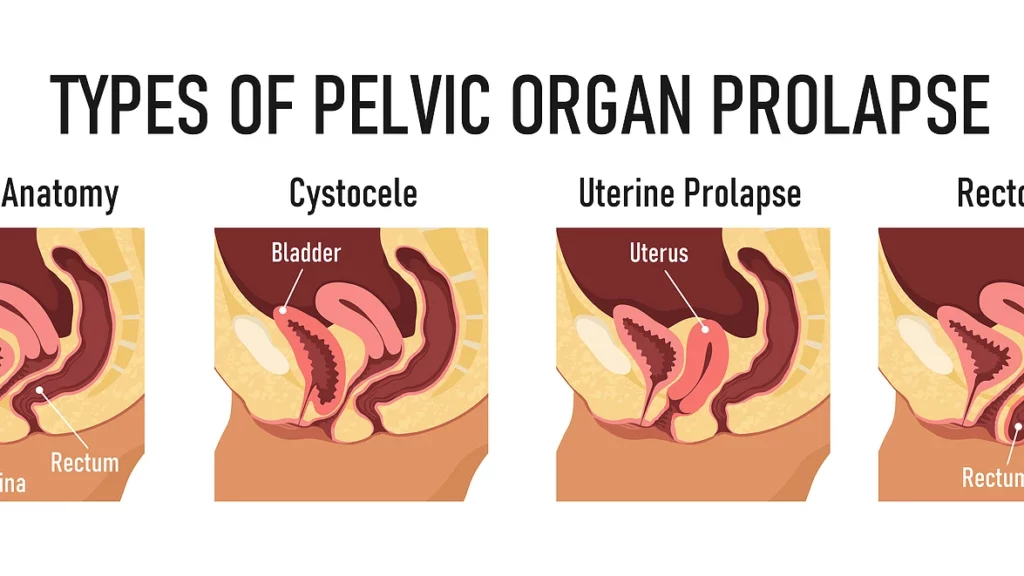
Under the umbrella term of “Prolapse” there are several different types, which typically depend on the location or organ where ligamentous support is lacking:
- Cystocele – bladder or anterior vaginal wall
- Urethrocele – urethra or anterior vaginal wall
- Urethrocystocele – urethra and bladder or anterior wall
- Uterine Prolapse – uterus or apex of vaginal canal
- Vaginal Vault Prolapse – apex of vaginal canal after a hysterectomy
- Rectocele – rectum or posterior vaginal wall
- Enterocele – large intestine or posterior wall
Who is more at risk for developing a Prolapse?
Pregnant women who push greater than 2 hours or less than 30 minutes, sustain any perineal tearing, lacerations or avulsions or have a forceps or vacuum delivery are all at an increased risk for developing a Prolapse after childbirth. Additionally, individuals who have undergone abdominal or pelvic surgeries, such as a cesarean birth or hernia repair, those who are diagnosed with a systemic disease or a connective tissue disorder, as well as those who suffer from chronic constipation with excessive straining are at an increased risk for developing a Prolapse. Lastly, those who repeatedly lift heavy for their job, regularly enjoy weight lifting for exercise or are prone to breath holding with any physical activity are at an increased risk for developing a Prolapse.
Common signs and symptoms of Prolapse?
- Vaginal Bulging – vaginal tissue coming to or past the opening of the vagina
- Feeling of pelvic pressure, heaviness or a “falling out” feeling
- Bleeding, Discharge or Infection – the vagina is lined with special tissue that is meant to stay inside the body. It may experience dryness, irritation or friction when exposed to air or rubbing against underwear.
- Low Backache – there are multiple ligaments connecting the digestive and reproductive organs to the sacrum and tailbone, therefore low back pain may be reproduced with excessive stretch and pull on these tissues.
- Splinting or Digitation – individuals may find the need to use their finger to support the vagina for urination or defecation
- Symptoms better lying down versus standing up or sitting
- Symptoms better in the morning, worse later in the day or after physical activity
- Symptoms more prominent after straining – i.e. constipation or heavy lifting
- Individuals may be asymptomatic and still have evidence of prolapse
What should you do if you suspect you might have a Prolapse?
When it comes to caring for your Prolapse, PRESSURE MANAGEMENT IS EVERYTHING! This means avoiding straining and breath holding as this places greater stress and pressure down on your pelvic floor, organs and their connective tissues.
If you struggle with constipation, try your best to manage this with proper water intake, diet and supplementation. Positioning is super important when it comes to DECREASING STRAIN during bowel movements, so try elevating your feet so your knees are above you hips when sitting on the toilet. (Check out my IG post on the squatty potty! https://www.instagram.com/p/CMTIHxLBZaV/?igshid=t3cbdbzc13w1)
With heavy lifting, be sure to utilize proper breathing mechanics so that you EXHALE ON EXERTION! This will help reverse the direction of pressure placing less stress downward on the pelvic floor.
Pelvic floor STRENGTHENING is important for increasing support of the organs and connective tissues. The pelvic floor is like a hammock at the bottom of your pelvis, and if that hammock is not strong or tied up well it tends to sag and not support what’s inside of it.
ADDITIONAL SUPPORT may also be necessary for those with prolapse. This may include trying internal vaginal support with use of a tampon or impressa, or eventually looking into a pessary for more long term use. There are also different external supports including various straps and undergarments on the market that may be beneficial.
Last, but not least SEE A PELVIC FLOOR PHYSICAL THERAPIST for more specific tips and tricks on how to manage your prolapse as well as to develop a home exercise program that is tailored to you and your specific needs. 🙂
For more information contact me via:
Email: hayley@fuelphysicaltherapy.com
Cell: (616) 274-0744
Instagram: @dr.hayleyvanbeek.dpt
Website: https://www.fuelphysicaltherapy.com/pelvic-pt-2021
Resources