Physical therapy is essential for restoring function and improving quality of life after knee replacement surgery. The recovery process following knee arthroplasty can be challenging, as patients must learn to overcome pain, muscle weakness, and limited mobility. Physical therapy in Grand Rapids provides a structured, evidence-based approach that supports healing while reducing the risk of complications, a methodology strongly endorsed by fuel health wellness. With targeted exercises and tailored treatment plans, physical therapists help patients regain strength, improve joint stability, and ultimately return to their everyday activities. For more information on personalized rehabilitation programs, please contact us. This article outlines the critical elements of physical therapy in knee replacement recovery and explains how carefully designed rehabilitation programs can promote quicker, more successful outcomes.
Key Takeaways
- Physical therapy after knee replacement is vital for regaining mobility, strength, and reducing pain.
- Customized rehabilitation programs focus on improving range of motion, muscle strength, and joint stability.
- Collaborative interactions with physical therapists and structured home-based strategies accelerate recovery.
- Optimal nutrition and overcoming common rehabilitation challenges further support healing post-surgery.
Understand the Importance of Physical Therapy for Recovery
Physical therapy is a cornerstone in the recovery process after knee replacement surgery, helping to re-establish movement and strength in the affected joint. Recognizing the importance of post-operative rehabilitation is essential because it addresses not only the physical setbacks but also the psychological challenges that accompany a major surgery.
Recognize the Benefits of Physical Therapy After Knee Surgery
Physical therapy offers numerous benefits following knee replacement. It improves joint mobility, enhances balance, and reduces dependency on pain medications. Patients who adhere to a structured therapy regimen often report a reduction in stiffness and an increase in their overall functional capacity. Studies have shown that those undergoing focused physical therapy recover faster and experience improved outcomes in terms of pain management and range of motion. Moreover, the constant guidance from a therapist builds confidence, which is crucial when learning to move again after surgery.
Identify Key Goals of Physical Therapy in Recovery
The primary goals in physical therapy after knee replacement include restoring the natural movement of the joint, rebuilding muscle strength, and ensuring proper gait patterns. These objectives are measured through various performance indicators, such as improved step lengths and increased quadriceps strength. Therapists set realistic short-term and long-term goals tailored to each patient’s condition. This systematic approach not only speeds recovery but also minimizes risks like falls or re-injury. In addition, targeted exercises help maintain flexibility in surrounding muscles, reducing compensatory movements that could lead to other joint issues.
Discuss the Timeline for Effective Recovery With Therapy
Recovery timelines vary from patient to patient, but physical therapy generally commences within days after surgery. Initially, the focus is on gentle exercises and pain management, progressing to more strenuous activities as healing permits. Within the first few weeks, therapy aims to decrease swelling and improve joint mobility. By three to six months post-surgery, patients typically notice significant improvements in muscle strength and an overall reduction in pain, though complete rehabilitation may continue for up to a year. A well-structured timeline allows for gradual intensification, ensuring that each stage of recovery is safely achieved while monitoring for setbacks.
Explore the Relationship Between Therapy and Pain Management
Physical therapy is not only about regaining motion; it is also closely linked with effective pain management. Early mobilization through guided therapy reduces inflammation and encourages the circulation of blood and fluids, which aids in pain relief. Techniques such as manual therapy, stretching, and the controlled use of modalities like heat or ultrasound help alleviate discomfort while fostering tissue repair. Additionally, tailored exercise programs empower patients to manage their pain better by strengthening the muscles around the knee, thereby reducing pressure on the joint and diminishing chronic pain potential.
Evaluate Progress During Therapy Sessions Accurately
Evaluating progress is a critical component of physical therapy. Therapists use standardized assessments to determine improvements in range of motion, strength, and functional mobility. Regular evaluations help in adjusting the exercise regimen to the patient’s evolving needs. This methodical monitoring provides both the therapist and the patient with tangible evidence of progress, which is motivating and essential for long-term adherence. Moreover, clear benchmarks and feedback allow for early identification of potential complications, ensuring that adjustments can be made promptly to avoid setbacks in recovery.
Learn Effective Exercises for Knee Rehabilitation
Engaging in a comprehensive exercise program is a crucial part of knee rehabilitation. Specific exercises help restore movement, build strength, and improve overall stability after knee replacement surgery. These exercises must be performed correctly and in a progressive manner to ensure optimal recovery while avoiding injury.
Incorporate Range of Motion Exercises Into Your Routine
Range of motion exercises are essential to maintain and improve the flexibility of the knee. These exercises typically include passive, active-assistive, and active movements that help achieve and maintain satisfactory joint mobility. Simple activities such as heel slides, ankle pumps, and gentle bending of the knee can prevent stiffness and encourage muscle activation. By gradually increasing the intensity and frequency of these movements, patients learn to perform day-to-day activities with less discomfort. These exercises are designed to stretch the joint gently while encouraging blood flow to the surgical site, which is crucial in reducing swelling and accelerating healing.
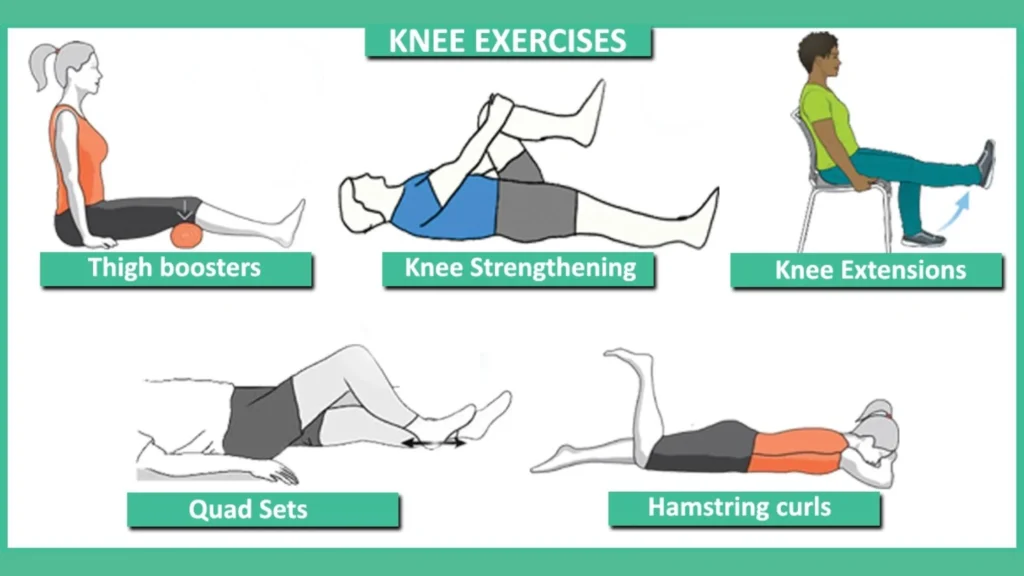
Practice Strengthening Exercises for Knee Stability
Strengthening exercises target muscles that support the knee joint, particularly the quadriceps, hamstrings, and calf muscles. Exercises such as straight leg raises, mini squats, and wall sits are often introduced early in the recovery process to rebuild strength without putting excessive strain on the replaced joint. The focus is on controlled movements that help in regaining muscle balance and stability. Over time, these exercises are progressively intensified to further enhance the patients’ leg strength and functional capability. Maintaining proper form during these activities not only optimizes recovery but also minimizes the risk of overloading the joint, thereby ensuring a smoother rehabilitation process.
Use Low-Impact Activities to Boost Recovery Safely
Low-impact activities are integral to knee rehabilitation because they provide cardiovascular benefits without placing excessive stress on the joint. Activities such as swimming, cycling, and using an elliptical machine help improve circulation, enhance muscular endurance, and promote overall fitness. These exercises are ideal during the later stages of recovery, where patients have already developed some degree of strength and mobility. The focus on low-impact workouts ensures that patients continue to build stamina and maintain an active lifestyle while protecting the new joint. Additionally, these activities support cardiovascular health, which is important for overall recovery and long-term wellness.
Adjust Exercises Based on Individual Progress and Needs
Personalization is key in the rehabilitation process. As every patient’s recovery trajectory differs, the exercise regimen must be tailored according to individual progress, strength levels, and pain thresholds. Regular assessments help in determining which exercises are effective and which may require modification. Therapists work closely with their patients to gradually introduce or intensify exercises as needed. Adjustments are made based on ongoing evaluations, ensuring that each person is challenged appropriately without risking injury. This dynamic adjustment process helps to optimize recovery and ensures that the therapy remains both safe and effective.
Seek Guidance on Proper Form to Prevent Injury
Proper form is paramount in physical therapy as it maximizes the benefits of each exercise while reducing the risk of injury. Under the supervision of a physical therapist, patients learn the correct techniques for every movement. Video demonstrations, hands-on corrections, and detailed instructions are commonly used to guide patients through exercises. Learning proper form early in the recovery process builds the foundation for safe, long-term practice. This emphasis on technique not only aids in effective rehabilitation but also educates patients on how to exercise independently after formal therapy sessions have ended. Consistency in proper form ensures that the healing knee is protected, and helps facilitate a smooth transition back to daily activities and physical activity.
Discover the Role of a Physical Therapist in Recovery

A physical therapist plays a pivotal role in designing and executing a recovery plan tailored to each patient’s needs after knee replacement surgery. Their expertise is crucial in assessing the patient’s condition, determining the most effective interventions, and providing ongoing support throughout the rehabilitation journey.
Understand How Therapists Develop Personalized Plans
Physical therapists begin by assessing the patient’s overall health, surgical outcomes, and functional limitations. Using this information, they develop a personalized plan that addresses specific deficits and targets areas that require the most work. These plans are designed to improve joint mobility, strengthen surrounding muscles, and increase overall stability. Personalized fitness programs are created based on objective assessments and are continually adapted to meet the evolving needs of the patient. This customization ensures that therapy is effective and minimizes potential risks or setbacks during recovery.
Collaborate With Therapists to Improve Motivation
The partnership between patients and their physical therapists is essential for sustaining motivation. Therapists provide not just physical guidance, but also emotional support during the recovery process. Regular sessions create an environment of accountability and encouragement, which significantly improves adherence to the exercise regimen. By setting realistic, measurable goals and celebrating incremental successes, therapists help patients maintain a positive outlook, which is key to overcoming the challenges of post-surgery rehabilitation. Effective collaboration ensures that patients remain committed to their recovery programs and steadily progress towards optimal functionality.
Explore How Therapists Adjust Plans Based on Feedback
Feedback from patients is an integral part of any rehabilitation program. Physical therapists actively solicit insights regarding pain levels, fatigue, and overall satisfaction with the exercise routine. This responsiveness allows them to adjust the treatment plan in real-time, modifying the intensity, duration, or frequency of exercises as needed. Adjustments are made to accommodate unexpected setbacks or to speed up progress when conditions permit. Patient feedback acts as an early warning system, highlighting issues before they escalate and ensuring that the therapy remains both safe and effective throughout the recovery period.
Identify Signs Indicating the Need for Therapy Intervention
Recognizing when additional intervention is needed is an important skill developed during physical therapy. Signs such as increased pain, swelling, or decreased range of motion may indicate that the current program requires modification. Therapists are trained to identify these indicators and implement immediate corrective measures. Early detection of potential complications can prevent further injury and ensure that the rehabilitation process remains on track. Consistent monitoring and evaluation enable therapists to address issues promptly, thereby reducing downtime and maintaining an effective pace of recovery.
Utilize Therapist Insights to Speed Up Recovery
Therapists not only guide exercises but also provide expert advice on various aspects of recovery. Their insights on ergonomic modifications, use of assistive devices, and strategies for pain management are invaluable in speeding up the rehabilitation process. By leveraging the professional knowledge of a physical therapist, patients can avoid common pitfalls and maintain steady progress. These expert recommendations often include detailed instructions on stretching, strengthening, and integrating physical therapy into everyday routines. Empowered by professional insights, patients are better positioned to achieve long-term recovery and return to their pre-surgery level of function more swiftly.
Optimize Recovery With Home-Based Strategies
Home-based strategies are equally important in ensuring a successful knee replacement recovery. While in-clinic physical therapy sessions play a crucial role, consistent practice at home reinforces progress and accelerates healing. Implementing an effective home-based program empowers patients to take control of their recovery and maintain momentum between clinical appointments.
Establish a Routine for Consistent Practice at Home
Developing a structured daily routine that incorporates rehabilitation exercises is vital for sustained progress. A consistent schedule helps to solidify the newly acquired movement patterns and reduces the likelihood of regression. Setting aside dedicated time for stretches, strength training, and balance exercises encourages patients to integrate therapy into their everyday lives. Over time, this consistent practice not only improves physical outcomes but also builds confidence in performing daily activities without external supervision. A well-planned home routine serves as a reliable framework, ensuring that therapy continues uninterrupted even outside the clinic setting.
Use Accessible Tools and Resources for Support
To maximize the benefits of home-based therapy, patients are encouraged to utilize various tools and resources designed to support recovery. Items such as resistance bands, stability balls, and foam rollers can significantly enhance the effectiveness of workouts when used correctly. Additionally, digital resources like online exercise libraries or mobile apps that track progress can offer guidance on proper form and timing. These accessible tools allow patients to perform exercises safely and effectively in the comfort of their own homes. The availability of such resources creates an enriched environment that fosters continuous improvement and ensures that therapeutic exercises are performed consistently.
Incorporate Stretches and Exercises Into Daily Life
Integrating simple stretches and exercises into daily routines can make a significant difference in long-term recovery. Instead of viewing physical therapy as a separate task, many patients benefit from incorporating movement into everyday activities. For example, taking short walking breaks, doing seated leg lifts while watching television, or performing gentle stretches during breaks at work can reinforce the benefits of formal therapy sessions. This seamless integration not only reinforces muscle memory but also prevents stiffness from prolonged inactivity. Over time, these small adaptations combine to create a comprehensive approach that bolsters recovery and improves overall physical health.
Create a Comfortable Environment for Recovery
The environment in which patients perform their home-based exercises plays an important role in their recovery. A well-organized, clutter-free area with supportive flooring and appropriate safety measures can reduce the risk of injury. Patients should ensure that they have ample space to perform each exercise with proper form. Additionally, a comfortable environment that includes motivational elements and proper lighting can help enhance focus and maintain enthusiasm throughout the rehabilitation process. Establishing a dedicated recovery space at home transforms therapy into a positive and accessible routine rather than a cumbersome obligation.
Monitor Improvements and Modify the Plan Accordingly
Regular monitoring of progress is essential for home-based recovery. Patients are encouraged to keep track of improvements in range of motion, strength, and pain reduction through journals or digital applications. This systematic tracking helps in identifying areas that require additional attention and confirms successful progress in others. Based on observed improvements or setbacks, the home exercise plan can be modified to either increase challenge or incorporate additional recovery modalities. Constantly re-evaluating the plan ensures that home-based strategies remain dynamic and continue to align with the patient’s evolving needs.
Assess the Importance of Nutrition During Recovery

Nutrition plays a critical role in the healing process after knee replacement surgery. A diet rich in essential nutrients supports tissue repair, reduces inflammation, and provides the energy needed for daily activities and rehabilitation exercises. The right nutritional choices can complement physical therapy efforts by accelerating recovery and improving overall surgical outcomes.
Identify Key Nutrients for Optimal Healing After Surgery
Protein, vitamins, and minerals are foundational to healing. Protein supports the repair of muscle tissues and is essential for rebuilding weakened structures around the knee. Vitamins such as C, D, and E, as well as minerals like zinc and magnesium, contribute to reducing inflammation and enhancing cellular repair. Omega-3 fatty acids, found in foods like fish and flaxseeds, are particularly effective in lowering inflammatory responses, which is crucial during the recovery phase. Ensuring that the diet is balanced and nutrient-dense can significantly contribute to faster and more robust healing.
Explore Supplements That May Aid Recovery Efforts
In some cases, supplements can provide additional support to the nutritional regimen during recovery. Supplements such as collagen, glucosamine, and chondroitin have shown promise in supporting joint health and improving cartilage function. These supplements, alongside vitamin D and calcium, are often recommended to support bone strength and strengthen the structures surrounding the knee joint. It is important, however, that patients consult with a healthcare professional before beginning any new supplements, as individual needs may vary based on overall health, medical history, and current medications.
Create a Meal Plan Focusing on Anti-Inflammatory Foods
An anti-inflammatory diet can be particularly beneficial after knee surgery. Emphasizing foods such as leafy greens, berries, nuts, and fatty fish helps to reduce systemic inflammation, which in turn minimizes pain and swelling in the knee. Incorporating whole grains, lean proteins, and a variety of colorful fruits and vegetables ensures that the body receives a broad spectrum of nutrients necessary for recovery. This approach not only supports physical healing but also improves energy levels and overall wellness, setting the foundation for a robust rehabilitation process.
Stay Hydrated to Support Healing and Physical Activity
Maintaining proper hydration is essential during recovery as water plays a critical role in every bodily function. Adequate fluid intake helps to flush toxins from the body, lubricate joints, and facilitate the transport of nutrients to tissues. In addition, hydration is crucial when engaging in physical therapy exercises, as it prevents muscle cramps and fatigue. Patients should be encouraged to drink water consistently throughout the day and consider hydrating beverages rich in electrolytes, particularly when engaging in exercise routines.
Discuss Dietary Adjustments With Healthcare Providers
Because nutritional needs can vary significantly among patients, it is important to tailor dietary choices to individual requirements. Healthcare providers and nutritionists can offer guidance on the most appropriate dietary adjustments during recovery. Through careful consultation, patients can develop a nutrition plan that addresses their specific health challenges, optimizes healing, and supports the demands of physical therapy. This collaborative approach ensures that the dietary component of recovery is aligned with overall therapeutic goals and contributes effectively to the rehabilitation process.
Understand Potential Challenges and Solutions in Recovery
Recovery after knee replacement surgery can be accompanied by numerous challenges that may impede progress. From issues such as persistent pain and inflammation to difficulties with motivation and adherence to exercise regimens, patients often face several obstacles. Recognizing and overcoming these challenges is a fundamental part of the rehabilitation process.
Acknowledge Common Obstacles in Knee Rehabilitation
Common obstacles in knee rehabilitation include pain, swelling, limited range of motion, and muscle imbalances. Patients can experience setbacks due to overexertion, improper exercise technique, or unrealistic expectations about the recovery timeline. Recognizing these challenges is essential for developing effective strategies to address them. Being aware of potential complications allows both patients and therapists to plan for and mitigate risks, ensuring that recovery remains on track. These obstacles, while daunting, can often be overcome with a carefully tailored and flexible rehabilitation plan.
Develop Strategies to Overcome Physical Limitations
To address physical limitations, therapists devise strategies that include modification of exercises, the use of assistive devices, and the incorporation of alternative therapies such as aqua therapy or electrical stimulation. These strategies aim to gradually build strength and range of motion while minimizing the risk of injury or re-injury. Special attention is given to muscle imbalances by incorporating unilateral exercises and corrective techniques that target neglected muscle groups. By providing personalized interventions and regular reassessment, therapists help patients overcome limitations and progress steadily toward full recovery.
Maintain Motivation Despite Setbacks in Progress
Recovery can be a long and frustrating process, and maintaining motivation is critical. Therapists work with patients to set realistic, incremental goals that provide a sense of accomplishment along the way. Regular progress tracking, positive reinforcement, and the inclusion of variety in the exercises help sustain interest and commitment. Additionally, support from family, friends, and fellow patients can play a crucial role in boosting morale. The structured feedback from professional assessments also reassures patients that their efforts are yielding tangible improvements, thereby reinforcing motivation despite occasional setbacks.
Utilize Support Systems for Emotional Well-Being
Emotional well-being is intrinsically linked to physical recovery. Psychological stress and anxiety can exacerbate pain perceptions and slow down the rehabilitation process. Support systems, including counseling, peer support groups, and regular check-ins with therapists, are vital for maintaining a positive outlook. A strong support network can provide emotional comfort and practical advice, helping patients navigate the challenges of recovery. Recognizing that recovery is not solely a physical journey, therapists encourage patients to focus on mental health strategies that complement physical therapy, ultimately resulting in a more holistic healing process.
Revisit Goals and Adapt Plans When Necessary
Recovery goals must be adaptable to account for individual progress and unforeseen changes in patient condition. Periodic reassessments allow for the adjustment of therapeutic goals, ensuring that they remain realistic and achievable. When patients experience plateaus or setbacks, revisiting and modifying the rehabilitation plan can reinvigorate progress and prevent frustration. Flexibility in the recovery plan is essential—it allows for the integration of new treatment methods or exercises as patients gain strength and confidence. Continuous adaptation of goals ensures that the therapy aligns with the evolving needs of the patient and that every aspect of the rehabilitation process is optimized for success.
Frequently Asked Questions
How soon should physical therapy begin after knee replacement surgery?
Physical therapy typically begins within a few days post-surgery to promote mobility and reduce swelling. Early intervention is crucial to prevent stiffness and initiate muscle strengthening.
What exercises are best during the early stages of recovery?
Early recovery exercises focus on range of motion, such as heel slides and gentle knee bends. These minimize stiffness and pave the way for more intensive strength training later on.
Can home-based exercises replace in-clinic therapy sessions?
Home-based exercises are an important supplement to in-clinic therapy, but professional supervision is critical initially to ensure proper form and progress.
What nutritional factors support optimal healing after knee replacement?
A balanced diet rich in protein, vitamins, and minerals supports tissue repair, while anti-inflammatory foods help reduce swelling and pain.
How do therapists tailor rehabilitation plans to individual needs?
Therapists assess each patient’s physical condition, progress, and pain levels, then personalize the exercise regimen and adjust therapy goals accordingly.
Final Thoughts
Physical therapy is a fundamental component in the recovery process after knee replacement surgery, ensuring that patients regain maximum function and return to daily activities swiftly. By integrating structured exercises, personalized treatment plans, and home-based strategies, recovery can be significantly optimized. Nutrition also plays a critical role in supporting tissue repair and reducing inflammation, further enhancing therapeutic outcomes. At Fuel Health Wellness, we provide expert physical therapy and wellness solutions designed to support recovery, promote strength, and enhance overall well-being. With consistent guidance, motivation, and adaptation to evolving needs, patients can overcome challenges and achieve a successful, lasting recovery.